Jo Mohan has lived with psoriasis since she was a baby. Now 41, she works full-time and runs a peer support group.... Read more >
Growing up with psoriasis: Mother and daughter share their stories
Growing up with psoriasis: Mother and daughter share their stories
Growing up with psoriasis was difficult for Karen Ridsdale. Watching her daughter deal with the pain and stigma of it was heartbreaking.
by Rosemary Ainley, 10 April 2022

Karen Ridsdale has lived with the skin disease, psoriasis, since childhood. She learned to deal with the social stigma and a limited range of smelly, greasy treatments. Yet, the hardest thing for her was watching her daughter, Sarah, grow up with a more severe form of the disease. Today, Karen is the President of Psoriasis Australia and a passionate advocate for people with psoriatic disease.
Karen’s journey
Karen developed scalp psoriasis when she was seven years old after a strep throat infection. Karen’s mother recognised the condition as it ran in their family and took Karen to a dermatologist for diagnosis and treatment.
In the second half of last century, psoriasis treatments were limited to topical products, cortisone (steroid) tablets or methotrexate (an immunosuppressive drug) to help manage symptoms.
Karen tolerated the topical products but did not like them as they were greasy and smelly. “I had the treatment on my scalp as that’s where it was more prominent,” she said. “My body image was horrendous. I’d put off doing it until Friday night and made sure that, by Monday, I didn’t smell so much of all the tar, my hair wasn’t greasy and I looked more ‘normal’,” she added.
Karen stuck with the treatments as she didn’t have much of a choice. “It was either go with the programs and use all the greasy creams or live with it being uncomfortable, itchy and painful,” she said. “However, if you have moderate to severe psoriasis today, you have so many treatment options that you never had before. I think that’s amazing.”
As a teenager, Karen found her psoriasis and treatments even more challenging. Finding shampoos and conditioners she could use was especially difficult. Hairdressers would suggest high-end products but they often contained ingredients that made her scalp psoriasis worse. Instead, Karen stuck to basic products she could trust.
Karen also tried dietary changes to see if that helped. “You’d spend a fortune trying holistic approaches like eliminating certain foods or adding vitamins and minerals. When you are young and want to be like everybody else, you do all these crazy things and then find that none of them work,” she said.
An ongoing frustration for Karen is unsolicited advice. “I know people are well-meaning and want to help but it’s usually non-medical advice that has no bearing on my condition. Often, the things they suggest would make my psoriasis worse,” she said.
Karen is also aware of the effects psoriasis has on relationships. “It’s not just about the person. It’s also about the impact it has on our partners, family members and friends,” she said. “For example, we have to think about getting to social events if we’re in the middle of a flare and we’re not looking or feeling the best. We need others to understand it’s not about them, it is about how our disease is impacting us at that moment”.
“We even have to think about having skin and blood on the sheets when we wake up in the morning as that can be difficult for a partner”.
Sarah’s journey
Karen’s daughter, Sarah, was diagnosed with psoriasis when she was two years old. “She had around 60 to 80 per cent of her body covered in different types of psoriasis,” Karen explained.
“Initially, Sarah’s treatments were the same tar-based ones I had when I was younger and it was difficult to watch her go through all that. I was disappointed that things hadn’t improved over that time,” said Karen.
When Sarah was a teenager, her psoriasis was very visible on her scalp, face, fingernails and other areas of her body. Karen said the psychological impact on Sarah as a young person affected her developing body image and sense of identity. “If you get it as an adult, you’ve already formed your sense of identity and know who you are as a person,” said Karen. “But if you get it when you are young, that ‘you’ is still formulating. So, when you look in the mirror and you see the effects of severe psoriasis, that messes with your head.”
Karen said this problem was made worse for Sarah at school. “When people bully or shun you because you’ve created a snowstorm of dry skin flakes around you — they don’t understand that it isn’t you,” she said. “It’s not the person. They have no control over it. It’s an autoimmune skin condition.”
Karen said that when Sarah went to nightclubs with her friends, they would tell her that boys liked her. “But she’d turn around and say (quite calmly), ‘Yeah, but they haven’t seen me in the daylight’”.
“Sarah might get a first date, but never a second date,” Karen continued. “She’d meet them for lunch in a café and they’d see it. They’d see the redness on her face, even though she’d done her best to hide it with makeup. There was no way she could hide all of it so she’d have to spend the first 15 minutes explaining what she had. It didn’t matter that she was a tall, gorgeous redhead with a great figure and personality. They couldn’t get past the skin”.
“She would just say, ‘If they can’t see me, that’s their problem’. But it hurt,” said Karen. “That’s why I feel for young people with psoriasis. I know the enormous impact our disease has on them. How they feel about themselves and how they see the world around them. Every time I see a young person struggling with this disease; I get to see that beautiful kid inside. I know how amazing, resilient and compassionate they are but other people are often shallow and don’t see that.”
Sarah’s working life was also affected by her psoriasis and fear of how others would react to it. Karen said Sarah was in constant fear of losing her job in hospitality. “She’d have long sleeves on and would go to wipe a table but she’d be worried someone would see her psoriasis and be disgusted by it. They might even think it’s contagious or ask her not to work there anymore.”
“Sarah did it tough but we got through it. There are impacts on her self-esteem that will never leave. As a mum, that’s heartbreaking.”
How biologic medications changed their lives
Tar-based products are still around but are less widely used. There are also other topical treatments available over the counter or by prescription, including cortisone-based creams. Many people with psoriasis also use methotrexate and cortisone tablets as part of their treatment.
Over the years, Karen developed guttate psoriasis and psoriatic arthritis (a form of autoimmune arthritis that is closely connected to psoriasis). She now regularly self-injects a biologic to suppress her immune system and manage both her psoriatic arthritis and psoriasis. “10 to 15 years ago we didn’t have those kinds of treatments. Then they developed biologics for rheumatoid arthritis and found they can work for us as well,” she said. “Now, we’ve got biologics that work for both psoriasis and psoriatic arthritis. Some work better for the skin and others work better for the joints but it’s great to have the choice.”
When biologics that targeted psoriasis become available, Sarah was keen to try one. She had a couple of options but chose the one she only had to inject every three months. “That fit in with her lifestyle,” said Karen. “They’re options we never had before.”
Within three months, Sarah was at the beach in a bikini for the first time in her life. “That was a very emotional thing for us,” Karen reflected. “She had completely clear skin within six months and we were all in shock. There were tears because, for the first time, my beautiful girl could be the beautiful girl we knew she was on the outside as well. There was no more recoil if people saw bare skin.”
It took a while for both women to adjust to life with clear skin, though. “It was quite strange,” said Karen. “We’d spent most of our lives camouflaging our psoriasis and not talking to others about it. Suddenly, we’re going down to the beach and wearing shorts.”

As president of Psoriasis Australia, Karen advocates for those with psoriatic disease.
About psoriasis
Psoriasis is an autoimmune disease that occurs when the immune system starts attacking healthy cells — usually skin cells — instead of targeting foreign bodies like bacteria and viruses. This process can cause skin cells to turn over much more quickly than usual (a few days instead of a few weeks).
The exact cause of psoriasis is not known but some people are genetically predisposed to it. In many cases, the genes remain dormant. However, they can become active following triggers such as stress or certain infections like strep throat. Risk factors such as smoking or obesity can also play a role.
Many people with psoriasis experience symptom flares that can last for days, weeks or even months and then subside again. It can occur on different parts of the body including the face, scalp, hands and feet, groin, skin folds and nails. Patches can be very dry, cracked and itchy but scratching can cause them to bleed. It can vary from mild patches in a few spots to severe cases that cover most of the body.
It is important to know that psoriasis is not contagious. You can’t catch it by touching someone else’s skin plaques.
Some people with psoriasis also develop psoriatic arthritis, a related disease that causes inflammation of the joints.

Sarah had psoriasis all over her body.

Having psoriasis on the face and neck often affects self-esteem.
Types of psoriasis
There are many types of psoriasis, including:
Plaque psoriasis is the most common form of psoriasis. Typical signs are thick patches of dead skin that usually show up on the elbows, knees and scalp, but can appear anywhere on the body.
When it appears on the scalp it is often mistaken for dandruff. The main difference in the appearance between dandruff and psoriasis is that dandruff is usually white, dry flakes, whereas psoriasis patches have a red or silvery sheen.
Guttate psoriasis looks different to plaque psoriasis. It is characterised by small red or brown scaly skin patches resembling drops and can occur anywhere on the body.
Inverse psoriasis can be mistaken for heat rash. Patches are flat, red and shiny and usually have defined shapes. It usually occurs in folds of the body, such as in the elbows, knees or groin.
Pustular psoriasis involves white, pus-filled, painful bumps often surrounded by inflamed skin. Palmar plantar psoriasis occurs on the hands and feet. Generalised pustular psoriasis is rare but can be life-threatening if not treated quickly as it affects vital functions.
Erythrodermic psoriasis is another rare form of the disease. Symptoms include intense redness and shedding of skin layers in large sheets. It often affects nearly the whole body and can also be life-threatening as it disrupts the body’s normal temperature and fluid balance.
It is possible to have more than one form of psoriasis at the same time.

Sarah is now proud to show her bare skin.
Psoriasis treatments
Common types of psoriasis treatments include:
-
Topical treatments such as emollients or cortisone creams.
-
Phototherapy or ultraviolet (UV) therapy mimics the beneficial effect of sunlight on psoriasis.
-
Medications to suppress the immune system. These include oral and biologic treatments. Biologics are administered via subcutaneous injection or infusion.
People with psoriasis are usually treated by a dermatologist.

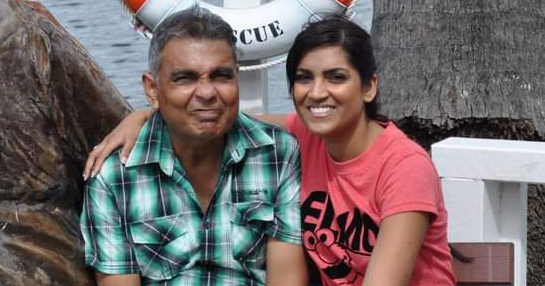
Mother and daughter promote the work of Psoriasis Australia.
Advocating for people with psoriasis
How treatment options are presented to people with psoriasis has also changed over time. Karen said the psychological and social impacts of using smelly, greasy topical treatments were never taken into consideration. “It was like, ‘This is what you have and this is the treatment option available to you’. You just had to do it. These days, patients are listened to and have a say in their treatment plan.”
Despite better treatments, anxiety and depression are still common amongst those with psoriasis. Karen says there is a lot of discrimination and stigma associated with the condition. As a result, many seek support through counselling and peer support groups.
As the president of Psoriasis Australia, Karen is passionate about making sure people with psoriasis are given a voice and supported. “We estimated with data from the World Health Organisation and the Skin Health Institute that there are around 1.6 million Australians with psoriasis.
She believes it is important to have a place where people can come for reliable information. “They can contact us and let us know what it is they’re struggling with and we’ll do our best to help them. We also advocate for more research funding for all forms of psoriasis,” she said.
“We want to help people come out from the shadows and be proud of who they are,” Karen added. “We don’t have to hide from other people. Most people with chronic illness are amazing, tough and resilient people. We need to celebrate that.”
If this article has raised feelings that concern you, visit the Lifeline website or call 13 11 14.
Psoriasis Australia
Email: [email protected]
Facebook: https://www.facebook.com/psoriasisaust
Twitter: https://twitter.com/psoriasisaust1
Website: https://psoriasisaustralia.org.au/
Sources
Mayo Clinic – Psoriasis: https://www.mayoclinic.org/diseases-conditions/psoriasis/symptoms-causes/syc-20355840
National Psoriasis Foundation – Locations and Types: https://www.psoriasis.org/locations-and-types/
Skin Health Institute – Psoriasis: https://www.skinhealthinstitute.org.au/page/97/psoriasis



Great article – describes the experience so well – it’s very hard to articulate. I have also passed it on to children and grandchildren. I found that the Dead Sea treatment was the only thing that helped ‘naturally’. Many other trweatments had unpleasant (or worse) side effects. I developed anxiety as a result and was reluctant to try new drugs. Still working through that.