Two new breakthrough treatments brings fresh possibilities for those living with chronic plaque psoriasis.... Read more >
My journey with psoriasis, psoriatic arthritis and peer support
My journey with psoriasis, psoriatic arthritis and peer support
Jo Mohan has lived with psoriasis since she was a baby. Now 41, she lives with several other autoimmune conditions, works full-time and runs a peer support group.
by Rosemary Ainley, 26 August 2022
Diagnosis and early treatment
When Jo was around six months old, she started to develop plaque psoriasis around her scalp. On doctor’s advice, her parents regularly applied a tar-based lotion to her affected spots. Jo’s father kept her hair short to help manage her psoriasis and people often mistook her for a boy. Having long hair like all the other young girls was what she always wanted.
No one explained psoriasis to Jo. She only knew applying the cortisone creams, scalp lotions and tar shampoos would help and that she had to try not to scratch the lesions as that would make them bleed.
Jo’s psoriasis started becoming worse when she was in high school. “I had big plaque patches on my arms that looked like burns as they were so red and sore to touch. It was even uncomfortable to wear clothes. Sometimes I wore looser clothing in the school colours rather than the uniform. Because my skin was always covered, no one knew about my psoriasis,” she said.
“I also started getting joint pain in high school. I used to play a lot of sports but started having pain and I didn’t understand why. I thought I was running around too much and it was just normal or growing pains. No one really explained that to me either,” she added.
Along with the joint pain, Jo also often felt tired and sometimes struggled to sleep. She spoke to her doctors about it for years but they couldn’t tell her what was causing it or they were dismissive. Some told her she was probably just overdoing things or that she had to live with it.
Psoriasis, self-esteem and worsening symptoms
Jo’s psoriasis had a big impact on her self-esteem. “Coming from a strict Fijian-Indian family, it was not like I could have boyfriends anyway, so it didn’t affect that. I would always cover up and not show a lot of skin. It hurt to touch my skin but sometimes you can’t help it. You don’t realise you’re scratching and then you start bleeding. I was very self-conscious of it and my self-esteem suffered.”
Jo had a boyfriend in her early twenties and she was paranoid about the effect of her psoriasis on her relationship the whole time. She would often feel ugly or unwanted. Around the time she was 23 her psoriasis kept getting worse. She went to a few dermatologists but all they did was confirm she had psoriasis and prescribe different or stronger creams. She recalls feeling that there had to be more she could do but she wasn’t getting any answers.

Jo in her school dress.

Jo with her cat Romeo who passed away last year.

Jo with her mum Devi and sister Arti.
Psoriatic arthritis appears
It wasn’t until Jo was 28 that a GP suspected she may have psoriatic arthritis (PsA) and asked if she had ever seen a rheumatologist. She hadn’t, so the GP referred her to one who diagnosed her with PsA and put her on methotrexate tablets to help all her symptoms.
Jo was also referred to a different dermatologist who was the best she’d ever met. These two specialists worked together to create her first treatment plan. Jo’s dermatologist also calculated Jo’s Psoriasis Area and Severity Index (PASI) score, which no one had done for her before. “I didn’t even know these things existed. At that stage, 80 per cent of my body was covered in psoriasis. I also had inverse psoriasis in my privates and my ears. My nails were all deformed and my scalp was pretty bad, it was one of the worst and most uncomfortable moments of my life.” she said.
Advanced treatments and new diagnoses
From there, Jo started a low dose of methotrexate and worked up to higher doses. However, she experienced some side effects so she asked if there was anything else she could try. She was amazed when they said yes and wondered why they hadn’t suggested it before.
Jo tried UV light therapy for a while. “I’m already brown and it gave me a really good tan, however, my skin reacted to it and it made my psoriasis worse so I stopped that,” she said. She also tried another oral medication without much success.
At that point, Jo was offered biologic medication and was approved for etanercept (which is a weekly injection). Her psoriasis and joint pain started to disappear within three to four months.
“It was the best feeling! I had never experienced not having to be itchy so I was happy to keep taking it. I did have some side effects when I took the injections. I would feel fatigued for about three days then have a few good days before taking it again. However, I thought if this is what I must do, then I’ll do it,” said Jo.
“It was good because my PsA was only in mild form and, because we got onto it early, it slowed the progression down a lot,” she added. “Once I got used to etanercept, it was fine. I was on it for about three or four years before it stopped being as effective for me. Then, I started methotrexate in injection form so, for a while, I was taking two different types of injections but that didn’t work. I’ve since been on several biologics and had different experiences with each of them.
After Jo moved cities, her joint pain started getting worse. She saw a new rheumatologist who diagnosed her with ankylosing spondylitis (AS). However, she stayed on the biologics prescribed by her dermatologist. Luckily, that biologic (infliximab) helped her psoriasis, PsA and AS.
Jo started having chest pain several years ago. She was especially concerned as several members of her family had died of heart disease. Her tests were all clear but her chest pain continued. “My cardiologist asked me if I thought it was anxiety but I didn’t think so because it didn’t feel like I was anxious,” said Jo.
“I went back to the rheumatologist and she suspected I had costochondritis (inflammation of the cartilage that connects a rib to the breastbone). I took anti-inflammatories and that worked for me. So now I have psoriasis, PsA, AS and costochondritis. I’m now on risankizumab for my psoriasis and PsA and I have it once every three months so it’s pretty convenient,” said Jo.
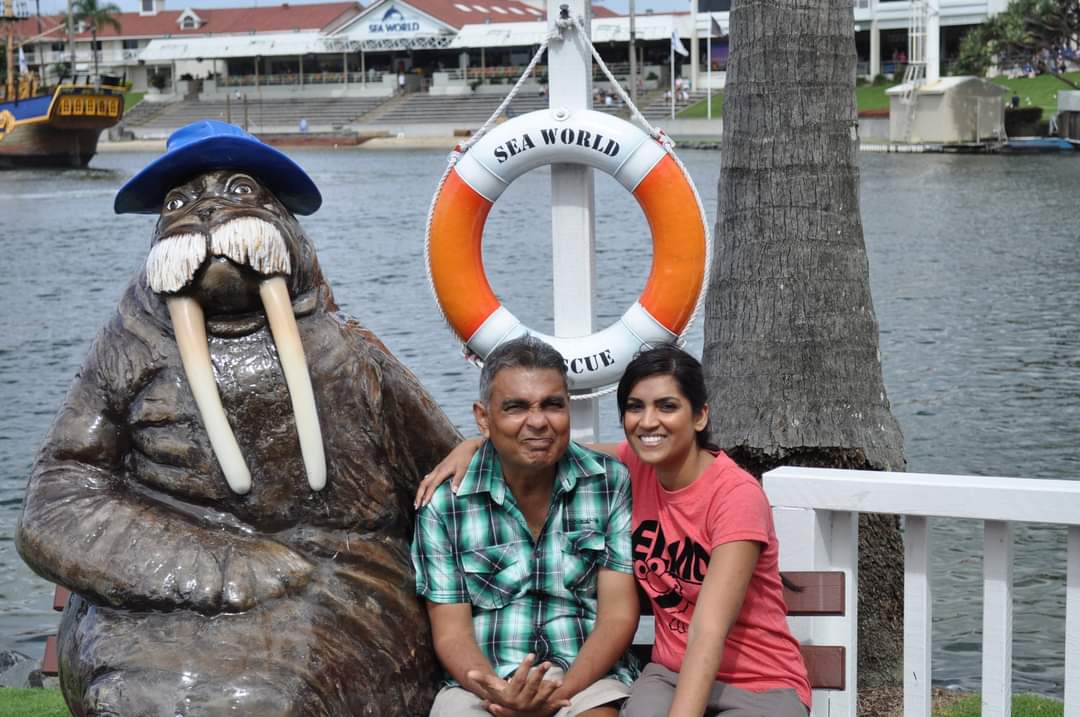
Jo with her dad Babu when he was unwell before he passed away, having a fun day out at Seaworld
Starting a peer support group for people with psoriasis and psoriatic arthritis
In 2011, Jo was at a low point. Her psoriasis and fatigue were bad and she had an inflexible manager at work so she resigned from that job. “I felt like I needed to give my body a break and I couldn’t keep working at that stage,” she explained. Her father also passed away in 2012, so she had a lot of stress in her life around that time.
“I was looking for support. My family are great, and they could see I was having a hard time but couldn’t help. I was struggling to explain what was going on. Even I didn’t understand what my body was doing or why it was doing it,” she said.
About psoriasis
Psoriasis is an autoimmune disease that occurs when the immune system starts attacking healthy cells — usually skin cells — instead of targeting foreign bodies like bacteria and viruses. This process can cause skin cells to turn over much more quickly than usual (a few days instead of a few weeks).
The exact cause of psoriasis is not known but some people are genetically predisposed to it. In many cases, the genes remain dormant. However, they can become active following triggers such as stress or certain infections like strep throat. Risk factors such as smoking or obesity can also play a role.
Many people with psoriasis experience symptom flares that can last for days, weeks or even months and then subside again. It can occur on different parts of the body including the face, scalp, hands and feet, groin, skin folds and nails. Patches can be very dry, cracked and itchy but scratching can cause them to bleed. It can vary from mild patches in a few spots to severe cases that cover most of the body.
It is important to know that psoriasis is not contagious. You can’t catch it by touching someone else’s skin plaques.
Some people with psoriasis also develop psoriatic arthritis, a related disease that causes inflammation of the joints.
Types of psoriasis
There are many types of psoriasis, including:
Plaque psoriasis is the most common form of psoriasis. Typical signs are thick patches of dead skin that usually show up on the elbows, knees and scalp, but can appear anywhere on the body.
When it appears on the scalp it is often mistaken for dandruff. The main difference in the appearance between dandruff and psoriasis is that dandruff is usually white, dry flakes, whereas psoriasis patches have a red or silvery sheen.
Guttate psoriasis looks different to plaque psoriasis. It is characterised by small red or brown scaly skin patches resembling drops and can occur anywhere on the body.
Inverse psoriasis can be mistaken for heat rash. Patches are flat, red and shiny and usually have defined shapes. It usually occurs in folds of the body, such as in the elbows, knees or groin.
Pustular psoriasis involves white, pus-filled, painful bumps often surrounded by inflamed skin. Palmar plantar psoriasis occurs on the hands and feet. Generalised pustular psoriasis is rare but can be life-threatening if not treated quickly as it affects vital functions.
Erythrodermic psoriasis is another rare form of the disease. Symptoms include intense redness and shedding of skin layers in large sheets. It often affects nearly the whole body and can also be life-threatening as it disrupts the body’s normal temperature and fluid balance.
It is possible to have more than one form of psoriasis at the same time.
Psoriasis treatments
Common types of psoriasis treatments include:
-
Topical treatments such as emollients or cortisone creams.
-
Phototherapy or ultraviolet (UV) therapy mimics the beneficial effect of sunlight on psoriasis.
-
Medications to suppress the immune system. These include oral and biologic treatments. Biologics are administered via subcutaneous injection or infusion.
People with psoriasis are usually treated by a dermatologist.
“I just wanted someone to talk to about it all. Someone who had been through and could tell me how they coped so maybe I wouldn’t feel so alone. I looked online for a support group and found one in America but I couldn’t find what I needed there.”
Jo decided to start something herself in the hope of finding others in similar situations. “I started a blog initially and wrote about my experiences and struggles. Then, I started a Facebook group (Psoriasis and Psoriatic Arthritis in Australia) in case there was another person sitting at home alone looking for help like I was. If they saw my page, they’d see at least one other person out there feeling the same way.”
“As hard as it was, I started sharing my story and putting myself out there,” said Jo. “I was a bit worried about what my family would think of it. What is she doing? Why is she sharing this personal stuff? But I did it anyway. What have I got to lose?”
Before Jo knew it, the support group started growing. People were contacting her, including people from the media asking her to share her story. “People have family and friends around them but it’s not the same sort of support as you get from talking to people that have been through something similar. The support and conversations are a bit different.”
“They can relate to things like trying to get ready for work. Sometimes it can be difficult because you can’t do it as your hands won’t function. A normal person wouldn’t think of things like that. They wouldn’t understand how frustrating it can be when you can’t do something simple like that,” said Jo.
Living with her chronic conditions
Jo now works full-time in a senior role. “My job is intense so it can be very draining. I struggle a lot with fatigue. That’s my biggest thing,” she said. “It can be hard if I’m working a 12-hour day and trying to manage my health. But working from home makes it easier. Having support and flexibility from others at home and work is very important.”
Jo has tried different forms of regular exercise to help manage her conditions. Walking and clinical pilates work best for her and they also help her mental outlook.
“If I can, I try to do my exercises in the morning,” she said. “Otherwise, if I wait until the end of the day, I’ve already used my energy up on something else. I don’t overdo it anymore. That took me a while to learn because I’d feel good then keep going. Then, I’d have to take two weeks off exercise to recover. So, I learned not to give it 100 per cent. Instead, I consistently give about 80 per cent.”
“I’ve also learned that you don’t have to be positive all the time. You’re allowed to have bad days and that’s fine. When I have a bad day, I used to feel guilty about it. Now I remind myself that it’s just a bad day and I’ll spend the whole day on the couch if I can. I’m not going to beat myself up about things like not working or exercising or about emotional eating on occasion,” she said.
“I remember talking to someone about choosing between what we’re happy to live with. The pain from something or the side effect from something. At the end of the day, you can never choose to be normal, it’s one thing or another. You just have to decide what to live with. Forget normal.”

Jo with her husband Kunal and dog Laila.

Jo in Istanbul where she attended a Psoriasis Patient Advocate Forum in 2013.
In 2017, Jo received a Healthy Skin Award from the Skin Health Institute for excellence in the promotion of skin health in the community. In the same year, she was also nominated for Australian of the Year by the Australia Day Council for her ongoing dedication and support to the psoriasis and psoriatic arthritis community.
Psoriasis and Psoriatic Arthritis in Australia – Closed Group
Facebook: https://www.facebook.com/groups/154849328409552
Sources
Mayo Clinic – Psoriasis: https://www.mayoclinic.org/diseases-conditions/psoriasis/symptoms-causes/syc-20355840
National Psoriasis Foundation – Locations and Types: https://www.psoriasis.org/locations-and-types/
Skin Health Institute – Psoriasis: https://www.skinhealthinstitute.org.au/page/97/psoriasis


This Post Has 0 Comments